Neurosurgical treatment of chronic pain (Medilife)
Postoperative chronic pain
This category includes a number of conditions such as the so-called failed back / failed neck pain syndrome. Many of these patients continue to suffer from pain, although clinical and imaging tests (X-rays, MRI scans, etc.) do not identify any cause of their pain. Implantation of spinal cord stimulators in the spine In […]
Post-traumatic pain
This describes the type of pain that persists after an injury, and is usually identified with neuropathic pain, i.e. pain that is not due to the injury itself, but to the chronic irritation of a nerve or nerves, and that lasts after the patient’s injuries have healed. Modern neurosurgery can help in the […]
Ghost member pain
This is a relatively rare disorder, attested in patients who have had a limb amputated, and after a period of time they start feeling pain in the missing limb. The mechanism of this disorder is not very well known, but it seems that it involves centers of the spinal cord and possibly the […]
Complex Regional Pain Syndrome
This is the name given to the syndrome that used to be called reflex sympathetic dystrophy and heartburn. There are 2 distinct types of this syndrome. In type I no nerve injury can be found, while in type II the nerve injury is given. It can occur in patients who have undergone an […]
Trigeminal neuralgia
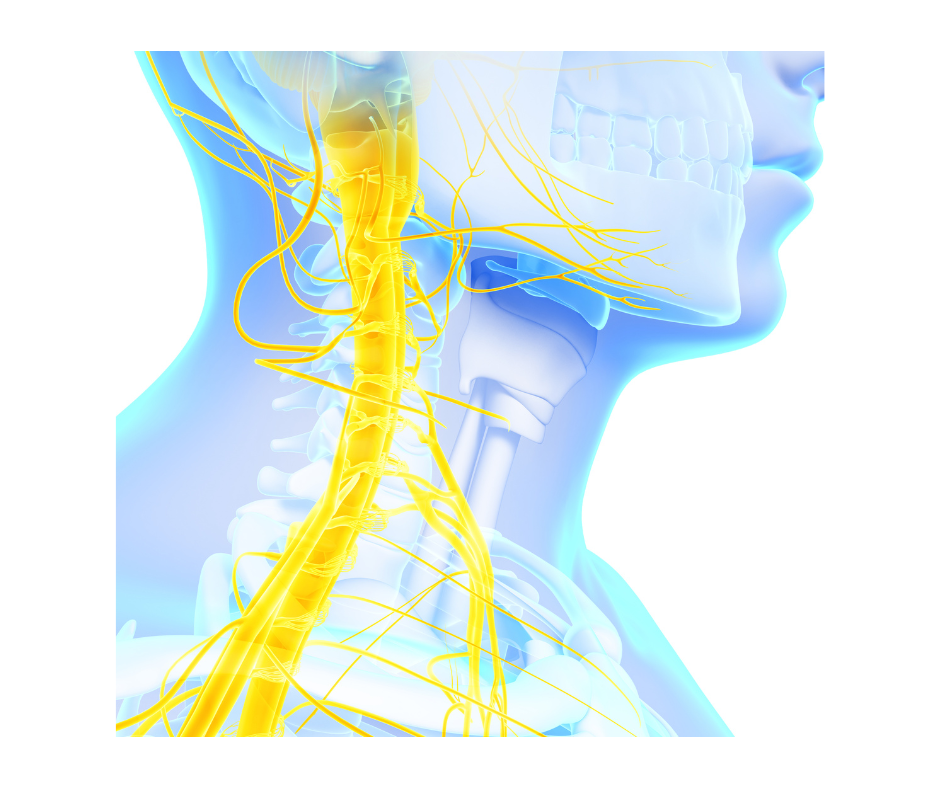
Trigeminal neuralgia is a neurological condition characterized by painful episodes involving the face. The pain is extremely sharp, it lasts for a few seconds, and it is often caused even by mild stimuli, such as chewing, smiling, touching the affected area, shaving, brushing your teeth, etc. Quite often, this is an unbearable pain that significantly […]

