Rehabilitation
What is rehabilitation? Rehabilitation is a process that requires the cooperation of physicians with different specialties, in order to restore the patient’s skills and help the patient’s family to adapt and help them cope with the consequences of their condition. The main idea for rehabilitation needs to be a rational approach to the improvements […]
Types of residual damage
Memory memory loss forgetfulness loss of train of thought inability to memorize instructions inability to complete a thought Spectrum of Attention difficulty concentrating easy distraction inability to focus when a competing stimulus coexists Reaction time slow reactions taking more time to think before answering Personality increased impulsivity reduction of inhibitions irritable, raising objections reduced […]
Recovery from coma
When the patient begins to wake up, the thought processes (cognitive functions) begin to become discernible and can be assessed. Patients usually wake up very gradually. Progress is made in slow steps that take time. Low-intensity controlled stimuli, such as speech, touch, sound, or visual stimuli, are more beneficial than longer stimuli, which […]
Stroke
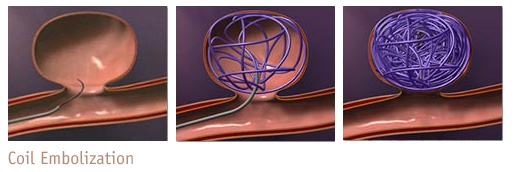
Ischemic stroke When a blood vessel in the brain is blocked by a blood clot or any other cause, normal blood supply to the brain is affected. Nervous tissue tolerates cessation of circulation for only a few seconds. The damage then becomes irreversible, and this part of the brain would have now suffered an ischemic […]

