Speech by neurosurgeon Nikos Maratheftis in Syros (Syros Today)
Event on Back Pain and Cervical Syndrome in Mytilene
Percutaneous spine surgeries
In modern surgery, with the help of technology and the accumulation of experience, new methods have been developed, which help surgeons perform operations that in the past were particularly traumatic, with minimal risk of surgical trauma. A typical example is spine surgeries, such as spinal fusion. Percutaneous spine surgeries significantly reduce patients’ […]
Pain Treatment with Radiofrequency Electrode Application
Radiofrequency therapy is indicated for the treatment of neuropathic pain, neuralgia, but also persistent musculoskeletal pain such as sciatica, low back pain and neck pain, which is continuous, has an anatomically clear distribution and is resistant to conservative treatment (medicines, patches, etc.). Neuropathic pain can be treated with the use of radiofrequency. Examples […]
Lumbar disc herniation – Spinal Stenosis: New Treatment Method
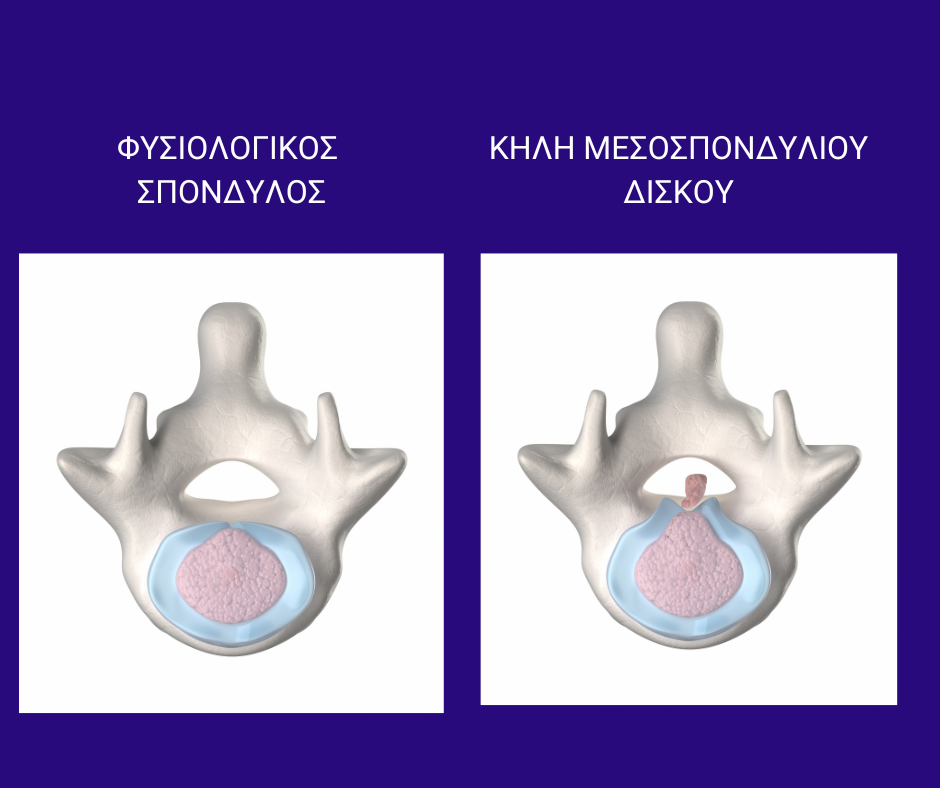
New treatment for back pain, sciatica and cervical syndrome
In modern medicine a new trend is developing in the treatment of diseases. These are new treatments for the most common health problems, such as back pain, sciatica and cervical syndrome . These treatments do not require hospitalization , they cost little and are just as effective as surgical procedures. Long-term medication in many patients […]

